

Trial registrationĬ identifier NCT03856528.
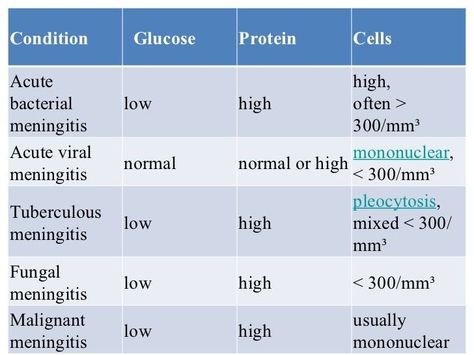
While increased CSF lactate and decreased glucose ratio are is the most reliable predictors of bacterial infections in patients with meningitis and/or encephalitis, only mononuclear cell counts predicted viral infections. Prior to microbiologic workup, CSF data may guide clinicians when infection is suspected while other laboratory and neuroradiologic characteristics seem less useful. All predictors revealed good calibration. While in multivariable analysis lactate concentrations and decreased glucose ratios were the only independent predictors of bacterial infection (AUROCs 0.780, 0.870, and 0.834 respectively), increased CSF mononuclear cells were the only predictors of viral infections (AUROC 0.669). Most frequent infectious pathogens were Streptococcus pneumoniae, Varicella zoster, and Herpes simplex 1&2. ResultsĪmong 372 patients, infections were diagnosed in 42.7% presenting as meningitis (51%), encephalitis (32%), and meningoencephalitis (17%). Calibration was defined as “good” if the goodness of fit tests revealed insignificant p-values. An AUROC between 0.7–0.8 was defined as “good”, 08–0.9 as “excellent”, and > 0.9 as “outstanding”. To quantify discriminative power, the c statistic analogous the area under the receiver-operating curve (AUROC) was calculated. Multinomial logistic regression was performed to identify predictors of the composite outcome. Meningoencephalitis was diagnosed if the criteria for meningitis and encephalitis were fulfilled. Infectious encephalitis was defined according to the International Encephalitis Consortium (IEC). Viral meningitis was diagnosed by detection of viral ribonucleic or deoxyribonucleic acid in the CSF. Infectious meningitis and/or encephalitis were defined as the composite outcome.įor diagnosis of bacterial meningitis the recommendations of the European Society of Clinical Microbiology and Infectious Diseases were followed. Clinical, neuroradiologic, and laboratory data were collected as exposure variables. MethodsĬonsecutive patients with meningitis and/or encephalitis form 2011–17 at a Swiss academic medical care center were included in this cross-sectional study. We aimed to determine predictors of infectious pathogens in the CSF of adult patients presenting with meningitis, and/or encephalitis. The purpose of this study was to explore the usefulness of BMS in South Korean patients, and to introduce BMS as a CPR.Cerebrospinal fluid (CSF) analyses are recommended in patients with meningitis and/or encephalitis, but evidence regarding its diagnostic yield is low. The BMS has been used as a guide in the Emergency Department to help exclude BM. A meta-analysis was also carried out in 2012 5).
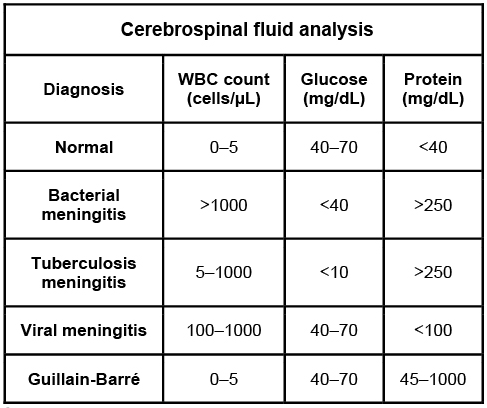
1), is the first validated model that was derived from a pediatric population in the postconjugate vaccination era and has been applied to the largest number of pediatric patients worldwide 1, 3, 4, 19, 20, 21, 22, 23). The bacterial meningitis score (BMS) 1, 5), introduced by Nigrovic et al. Many researchers have investigated several clinical prediction rules (CPRs) to discriminate these two etiologies. Unfortunately, there is not currently a single clinical symptom or laboratory finding that distinguishes BM from AM. This overuse of medicine not only increases the risks of patients developing adverse effects to treatment and acquiring nosocomial infections, but also is wasteful in terms of medical cost. In most cases, this means that patients are treated with antibiotics and are hospitalized unnecessarily. Given the similar presentations between BM and AM, most pediatricians empirically treat with parenteral antibiotics for two to three days until negative culture results rule out BM 4, 18).


 0 kommentar(er)
0 kommentar(er)
